Surprisingly, refugee camps across the globe have not seen the mass COVID-19 infections initially projected by health officials. Given the poor conditions in refugee camps, including overcrowding, poor sanitation, and frequent close contact among residents, how is that even possible? For potential answers, we can turn to a camp for migrants in Matamoros, Mexico.
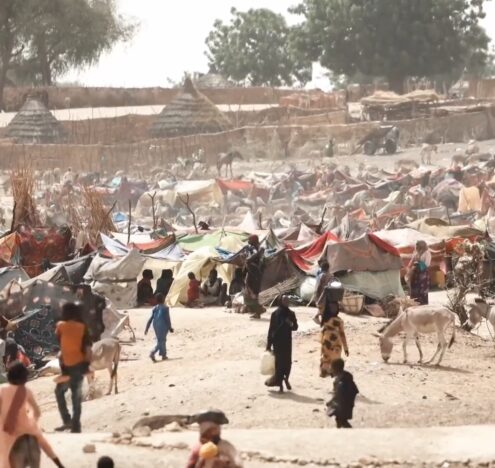
Currently, there are about 2,000 migrants living in the camp. The majority are fleeing cartel violence in the Central American Triangle, but also include Venezuelans, Haitians, and internally displaced Mexicans. Rather than a permanent settlement, the camp is intended as a stopping point for migrants hoping to receive asylum in the United States. The unfavorable immigration climate under President Trump deterred migrants from seeking asylum in the United States. Under President Biden, migrants believe that their chances of acceptance are much higher, and are arriving at the border, and the camp, in greater numbers.
As a result, the small non-profit organization that runs the camp, Global Response Management (GRM), is spread thin both in terms of personnel and resources. They have only a 14 person permanent staff that is responsible for operations in six countries worldwide. Nonetheless, the non-profit’s COVID-19 response in February 2020 was centrally-coordinated and swiftly administered. As of February 2021, their pandemic protocol continues to reflect the latest recommendations by leading scientists.
As part of their prevention strategy, GRM built a fence around the camp, with one entry point and mandatory temperature checks. Staff quickly established an isolation area and field hospital, equipped with an X-ray machine and ultrasound, where rapid antibody and antigen tests were administered to camp residents. They also added additional charging and clothes-washing stations to prevent crowding and facilitate social-distancing. From 6 a.m. to 10 p.m., a team decontaminates all high-touch surfaces in the camp every 30 minutes, including restrooms, hand sinks, and aqua blocks. In addition, all camp residents have access to masks and a 24-hour medical hotline.
GRM’s immediate strategy was so effective that COVID-19 only appeared in the camp for the first time in June 2020. That remarkable fact stands in stark contrast to the city of Matamoros just beyond the camp’s barriers, where 25 cases were recorded as early as March 18, 2020.
Refugee camps’ same pattern of success exists when we control for population size. In Cox’s Bazaar, a refugee camp for Rohingya Muslims in Bangladesh run by the UNHCR, the first case of COVID-19 was reported on May 14, 2020, almost two months after the virus first arrived in Cox’s Bazaar District. That is particularly remarkable considering that Cox Bazaar is the largest refugee camp in the world, with more than 600,000 people living in an area of just 13 square kilometers.
Refugee camps have fared extremely well against COVID-19 because they operate through the lens of humanitarian assistance.
Refugee camps have fared extremely well against COVID-19 because they operate through the lens of humanitarian assistance. Camps are set up to provide protection to people fleeing from the world’s greatest humanitarian emergencies. In order to best protect migrants, organizations running those camps must quickly adapt to shifting conditions on the ground, and develop contingency plans to address potential issues.
The protection of human rights is also central to those organizations. Migrants arrive at camps after enduring various forms of trauma. Organizations are aware of the psychological as well as physical strains on migrants, and provide services designed to mitigate the harsh realities faced by migrants. Because the human rights of migrants are central to organizations like GRM, they had to be forward-thinking and swift in their response to the pandemic and other threats to the well-being of migrants. Andrea Leiner, Director of Strategic Plans for GRM, explained to me that GRM’s swift response came out of a fear of the “vulnerability” of camp residents to the virus.
The lessons from GRM’s approach to the pandemic, with its emphasis on treating people’s well-being as its central focus, should be followed by developing and developed nations alike. Such an approach would likely have resulted not only in fewer infections, but also a more holistic approach to social well-being.
The Mexican government did not take such an approach, to the detriment of their citizens. Although the percentage of the population currently COVID-positive in the city of Matamoros is lower than that in the camp, at 1.4%, outcomes for sick people are markedly worse. Public and private hospitals refused to accept people with COVID, resulting in at least 20 people dying in their homes or on streets outside the hospital. Five hospitals that serve a population of 541, 979 people, 7,532 of whom are COVID-positive, only have 111 beds for COVID patients. It is also suspected that the number of COVID-positive people is a gross underestimate due to a myriad of factors, including the lack of testing and contact tracing, and a historic fear of the healthcare system.
Furthermore, there is no free COVID testing in Matamoros outside the refugee camp. Salud Digna, a Mexican clinical laboratory, charges $250 MXN for an antigen test and $950 MXN for a PCR diagnostic test. The average salary in Matamoros is $5,760 MXN a month. One antigen test constitutes 4% of a person’s monthly salary, and a PCR test 16%; a test is therefore beyond the means of a significant portion of the population.
The dire situation in Matamoros is the result of a reactive, rather than proactive, response on the part of the national and local governments. The rollout of a comprehensive plan was seriously hampered by a lack of leadership on the part of President López Obrador, and the Ministry of Health. Once the virus had already arrived in Matamoros, Municipal President Mario López urged citizens to wash their hands with soap and water for 30 seconds, use antibacterial gel with 70% alcohol, cover the nose and mouth, and avoid hugging and kissing. Notably, there were no plans in place to address the imminent healthcare crisis that was already spreading in the city. By placing the burden of mitigating the spread on individual citizens, the state essentially deflected responsibility. Instead of developing infrastructure that would have saved lives to address the public health emergency, the state implemented policies on a piecemeal basis.
To be sure, managing a small, confined refugee population with minimal political issues to address and no economy to worry about is very different than managing a city. However, the responsibility for a community’s well being rests squarely on the shoulders of governing bodies, whether they are in charge of a relatively small camp for migrants or a large city.
Taking a crisis oriented mindset, and centering people’s rights and wellbeing, should be the guiding principle moving forward. After all, the next pandemic is likely right around the corner.
Anna Braverman is a Master’s student at The Fletcher School of Law and Diplomacy specializing in human security and public international law. Previously, she served as a Fulbright scholar to Mexico.